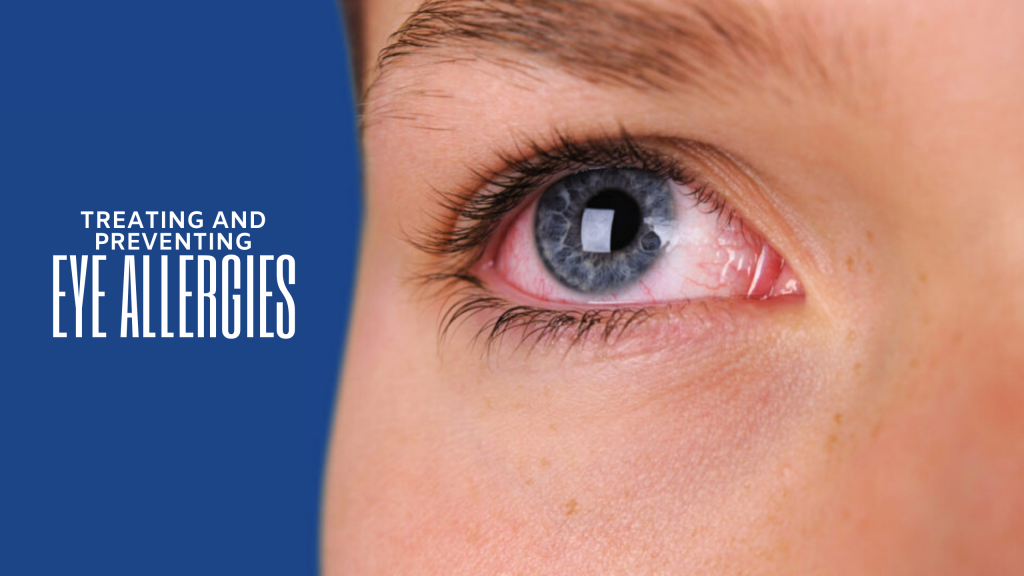
When patients approach us about eye allergies, their symptoms typically include swelling (puffy eyes), redness, itching in addition to watery eyes and/or mild yellowish stringy mucous discharge from the eye.
As eye doctors, the most common signs we see are erythema (redness) and edema (swollen eyelids), periorbital area, and conjunctiva (pink eye). Specifically, the conjunctiva may show an injection of the blood vessels (red eyes), a papillary reaction (similar to hives but in the eye), and/or conjunctival chemosis (swelling of the white part of the eye).
These symptoms and signs typically appear after immediate physical exposure to an allergen—however, the reaction can be delayed for two to three days after the initial event of exposure. So you may be unclear about what caused the allergic reaction.
The most common outdoor allergen is pollen. For our patients in Georgia, primary pollen producers include ragweed, hay, and various grasses. With oak, cottonwood, hickory, sycamore, elm, juniper, pecan, walnut and willow as secondary producers.
Indoor allergens that cause eye allergies are dust mites, pet dander, mold, clothing detergents, old pillows, old bedding, and/or poor replacement schedule of AC unit filters. Other known irritants include second-hand smoke, perfumes, and vehicle exhaust.
In some cases, contact lenses may be the source of the allergen. Many people develop an allergic response to contact lens material, such as silicone hydrogel or hydrogel. This diagnosis is called Giant Papillary Conjunctivitis (GPC). Monthly or two-week replacement contacts present a greater opportunity for eye allergies to develop in comparison to daily replacement contact lens. When the same contact lens is used repeatedly over several days, it will accumulate and absorb debris similar to a sponge. That debris commonly causes the ocular tissue to slowly or suddenly develop allergies. Contact-based allergies can be avoided through switching to daily replacement contact lenses, improving contact lens hygiene, or switching contact solution brands. You should always consult your eye care physician before changing solutions or contact lens brands.
The best way to prevent the symptoms of eye allergies is to avoid exposure to known allergens or pre-treating your eyes before exposure to them. This may include keeping windows closed during high pollen periods, wearing glasses or sunglasses when outdoors, using mite-proof bedding and covers, using a dehumidifier to control mold, and washing hands frequently when handling pets.
Proactive pre-treatment is a targeted approach to avoid symptoms of eye allergies. We educate our allergy-prone patients to be more aware of their allergy triggers. When they know they’ll be in contact with a known allergen, they can pre-apply topical antihistamine eye drops and/or oral antihistamines may suppress the allergic response.
Then after the exposure, we recommend they flush their eyes with preservative-free artificial tears in addition to washing hands, face, clothes, body, etc. This will remove any possible lingering allergens.
There are a variety of ways to treat ocular allergies, both mild to chronic cases, once the symptoms have appeared. For best results, speak to your doctor about the best treatment option for you. One thing to note: eye rubbing should be avoided at all costs, as this can actually make symptoms worse. The following are common courses of treatment.
The first-line therapy for the treatment of ocular allergies includes OTC eye drops. These eye drops can be as simple as preservative-free artificial tears or topical antihistamines eye drops such as ketotifen. Fair warning, drops containing decongestants should be avoided due to concern over rebound hyperemia. These eye drops include naphazoline, oxymetazoline, or tetrahydrozoline.
Cold compresses to the surrounding ocular tissue and even refrigerating eye drops may give an additive therapy to reduce associated swelling and inflammation of the ocular tissues.
Prescription medications may be needed in moderate to severe cases. Topical prescription antihistamines such as bepotastine or olopatadine may be indicated if over the counter ketotifen cannot adequately suppress the symptoms. Topical antihistamines can be tolerated for longer periods of times with minimal side effects.
One common low-grade side effect of antihistamine use is dry eye. You may want to consult an eye care physician before use to determine if antihistamines will worsen your dry eye symptoms. The side effects of dry eyes are typically mild and can be halted by discontinuation of the antihistamine. Although these topical antihistamines are typically a more effective therapy, insurance coverage is minimal.
A less conservative approach includes the use of topical steroids, such as loteprednol, fluorometholone, prednisolone, or dexamethasone. Topical steroids are very successful in the short term treatment of ocular allergies, but they should only be used sparingly due to their long-term side effects. Long-term side effects of topical steroids include raised intraocular pressure and cataracts.
These side effects typically develop with prolonged usage, high dose usage, or self-directed usage by the patient. We always recommend that patients only use steroids as directed by their doctor (in terms of both duration and dosage) and to return for follow up in order to minimize these unwanted side effects. A common approach is to first use a topical steroid to control the symptoms of ocular allergies. Then after tapering off the steroid, we recommend transitioning into topical antihistamine use daily to maintain suppression of the symptoms. This method tends to avoid the long-term side effects associated with topical steroids.
Other known therapies for ocular allergies include oral antihistamine use such as cetirizine, loratadine, or diphenhydramine. When using oral over the counter products, we suggest that patients always consult their internist or primary care doctor before usage. In addition to over the counter oral medication, over the counter corticosteroid nasal sprays may help to suppress the symptoms of ocular allergies. Since the nasal tissues are adjacent to the ocular tissues, treating both together can be an additive therapy for desired relief.
When all else fails to suppress ocular allergies, patients may need to seek consultation with a local allergy specialist. These doctors have the ability to identify your sensitivity to allergens by allergy testing, as well as prescribe systemic medications to suppress and potentially cure the symptoms of ocular allergies.
Contact us to discuss your treatment options and schedule an appointment today!
Schedule an Appointment Online
Or call 678-381-2020