Glaucoma is the second leading cause of blindness worldwide. In the United States, primary open-angle glaucoma (POAG) is the most common form of glaucoma and is the leading cause of irreversible blindness in African Americans. Unfortunately, the disease process is asymptomatic until advanced loss of peripheral vision occurs very late in the disease. There are no visual changes, no pain, and no redness that occurs in POAG. It can only be diagnosed, and treated, with a thorough examination by an eye doctor. The precise mechanism of the disease is poorly understood. However, certain risk factors have been identified through numerous studies which include: Advancing age, positive family history, African American ancestry, thin corneal thickness and myopia. The good news about POAG is that it is one of the most prominently studied diseases in eye care. The treatment options are getting better and more efficient with time.
Description
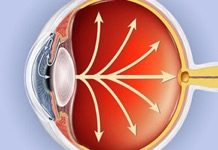
Primary Open Angle Glaucoma is a condition in which the optic nerve is damaged. This damage is indicated by characteristic cupping of the nerve and thinning of the neural rim of the nerve itself. The characteristics of the disease process are indicated by increased intra-ocular fluid pressure, an open drainage system for the fluid to flow, and progressive damage to the nerve tissue. In the early stages of the disease, there are absolutely no symptoms. As the disease progresses into the later stages and the optic nerve suffers progressive damage, the patient may begin to notice peripheral vision loss. For instance, the patient may not be able to see a car coming up beside them on the highway. Or, they may not see the curb or step in front of them and this may lead to falls. Unfortunately, by the time the patient begins to have these types of symptoms, the disease has progressed significantly. Typically, early treatment intervention can prevent the patient from progressively losing their peripheral vision. However, treatment needs to be started early. Once the neural tissue is damaged, it is cannot recover. This is why it is so important for everyone to have a dilated, comprehensive eye examination at least once per year.
Progressive Optic Nerve Cupping in POAG
Risk Factors
Intra-ocular pressure (IOP) is the most important risk factor and the only modifiable risk factor. Numerous studies throughout the world have proven that with increased IOP there is an increased risk of progressive cupping.
Several studies have shown POAG to be more prevalent in patients with African-Carribean descent compared with Caucasians. Studies also show that the onset of the disease is earlier, and the progression is faster. Hispanic patients have prevalence somewhere between Caucasian patients and those of African descent.
Several large studies have found that the prevalence of POAG increases with age. And, a person with a first degree relative who has POAG is at a higher risk of developing the disease. Furthermore, the risk goes up even higher if that relative is a sibling.
Diagnosis
The diagnosis of POAG is not made in one visit to an eye doctor’s office. Think of it this way, establishing the diagnosis of glaucoma is like putting a puzzle together. There are several pieces of the puzzle that must fit together in order to make a “clinical picture” of glaucoma. If there are only a couple of pieces that fit, (i.e. family history and increased intra-ocular pressure) but everything else is normal, (i.e. optic nerve, visual field, etc.) then more data will need to be obtained before a true diagnosis of POAG can be made. This may entail numerous office visits, pressure checks and visual field tests.
The gold standard for testing the intra-ocular pressure is by Goldman Applanation Tonometry. In this test, the doctor or staff technician will put drops in the patient’s eye to anesthetize it. Then a probe, connected to the slit lamp, will be used to gently read the pressure inside the eye by applying it to the cornea. We know from numerous studies that the intra-ocular pressure in the human eye fluctuates diurnally. That is to say, it is highest in the early morning hours and lowest in the late afternoon hours. This is important because we need to establish a peak pressure before we can determine future treatment strategies.
Clinical examination of the optic nerve is the most important diagnostic test to determine whether a patient has glaucoma. This requires dilation in order to be done accurately. The doctor can see the optic nerve with high magnification by using condensing lenses while looking through the slit lamp. If the doctor determines that the optic nerve is suspicious for glaucoma damage, further testing is needed.
Some of the tests that can be helpful in determining whether there is glaucoma damage to the optic nerve are OCT, HRT and GDX. All of these are sophisticated machines that use high resolution imaging to determine the thickness of the retinal tissue around the optic nerve as well as the amount of neural tissue remaining in the optic nerve. Another important test is high powered photographs of the optic nerve. These can be used to determine future changes to the tissue and subsequent progression of the disease.
Gonioscopy is a test where the doctor holds a hand held lens on the front of the eye and looks into the lens to determine whether or not the drainage system of the eye is open or narrow, clogged with debris, or if there is scarring or new blood vessels growing where they should not be.
The visual field test is one of the more important tests used not only to diagnose glaucoma but, more importantly, to monitor the progression of the disease. In this test, the patient looks into a machine which has a white screen. As the patient fixates on a central light, small lights are flashed in the periphery. When the patient sees a flash of light, they push a hand held button. This not only determines the scope of the peripheral vision but also the depth of the defective areas in glaucoma visual field loss. Multiple tests are usually needed before a diagnosis of POAG can be made and multiple tests are needed per year to determine the effectiveness of treatment.
Treatment
There are several treatment strategies to save the vision in a patient with POAG. The first is topical medications. Most first-line treatment medications only have to be used once per day. Some have to be used twice per day.
Laser treatment may be a possibility in some patients with POAG. The new lasers used today are effective and repeatable as their effects usually only last a few years. This can be used in conjunction with topical medications or as a standalone therapy.
If topical and laser therapy alone are not sufficient to lower the pressure and stop the progression from POAG, oral medications can be added. However, as with any medications, these may carry some side effects. Your doctor will determine whether or not this treatment would be right for you.
Surgical therapy is a fast growing and changing treatment strategy. Minimally Invasive Glaucoma Surgery or MIGS is a popular treatment option amongst doctors because these procedures are, as described, minimally invasive, and most can be done in conjunction with cataract surgery. We will discuss these in detail at a later time. A more invasive type of surgery is called a trabeculectomy. This surgical procedure is much more invasive, is highly unpredictable, and is usually reserved for those patients for which all other treatment strategies have failed.
Conclusion
If left untreated, POAG is one of the few conditions that can lead to irreversible and complete blindness. However, studies show strong evidence that aggressive lowering of the intra-ocular pressure in a patient can stop, or at least, slow the progression of the disease so that a patient will retain their functional vision and live a normal happy life. Because there are no signs or symptoms of early POAG, it is very important for everyone, especially, if you are over 40, to have a comprehensive dilated eye examination every year.
Make an appointment today at one of our eight convenient Atlanta-area locations.
Schedule an Appointment Online
Or call 678-381-2020